How Newcastle dental researchers are saving smiles
Read our interview with Newcastle graduate and Clinical Fellow at our School of Dental Sciences, David Edwards, to discover the current revolutionary research led by our alumni to tackle tooth pain tormenting millions of people a year.
2 September 2025
Dental education began in Newcastle in 1895. For the past 130 years, our School of Dental Sciences has trained dental professionals to care for patients around the world, and research the biggest issues in the field. Today, it is one of the largest and best equipped dental schools in the UK.
Currently, alumni researchers based at the Dental School are developing revolutionary cellular models to test different treatments for one of the biggest issues faced by patients (and one of the most under-researched areas of dentistry): toothache!
To mark World Smile Day (3 October), we spoke to Newcastle University graduate and Clinical Fellow at our School of Dental Sciences, David Edwards (BDS, 2005), to hear more about his plans for preventing phantom tooth pain, his memories of Newcastle in the early Noughties, and where his career has taken him since – from the army to operating on sloths!
Nurturing the next generation of Newcastle dentists
I first arrived on campus in September 2000 as a Fresher and spent my first year at Castle Leazes. It’s funny to now be working every day in the hospital just over the road! I immediately felt at home in Newcastle, all the staff I interacted with as a student were approachable and caring. In my role as an educator today, I try to spread that ethos and provide a nurturing environment to the next generation of Newcastle dentists.
The friendships I made in my first year on campus are still going strong, over two decades later. We all made sure to socialise outside of our studies, and DentSoc nights out on a Friday were a big part of my student experience. We even went out the Friday before our finals!
I was also involved with the University’s bowling team and Mountaineering Society, with lots of fond memories of camping in Scotland, and I started a dentistry football team which is still going strong today! It always makes me smile when tutees come to me to say they’re part of the Axe-Wielding Baboons, and I get to inform them I’m the founding member.
After graduating, I stayed in Newcastle for two years before joining the army – which I was part of for 12 years. If there was ever anywhere I was going to come back to, though, it was Newcastle. I returned to the Dental School in 2019 and lecture on endodontics, anatomy and neuroscience.


The diagnosis all dentists dread
It’s fair to assume that anyone reading this has had tooth pain at some point in their life, or the associated jaw and facial ache. It’s one of the most common reasons people visit their dentist, with a reported 2 million people in the UK getting toothache a year. And yet, when a patient sits down and says they’re suffering with this type of pain, as a dentist your heart sinks. Because despite it being so common, the causes of this pain are severely under-researched, and so we really are at a loss on how best to treat you.
The most common treatment for consistent tooth pain would be removing the tooth, or removing the nerve from within the tooth (root canal). These procedures are done routinely, but there’s been no evidence to suggest it actually works in resolving the issue, and in fact, a small but important proportion of patients can have one of these treatments and then go on to suffer from phantom tooth pain or Temporomandibular disorders (TMD). TMD has several different subtypes with one of the most common being constant jaw muscle pain. With no high-quality evidence available to help guide specialists’ decisions on treatment options, up to 49% of people with TMD currently suffer life-long pain.
To combat this issue, Newcastle University have launched the world’s largest ever trial into TMD, with the MiTiGate trial recruiting patients until summer 2026. At the same time, fellow Newcastle Dental graduate Professor Justin Durham and his team here on campus led NHS England’s national guidelines for the disorder and instituted a nationwide care pathway.
TMD affects up to 1 in 15 people, categorically worsens quality of life and interferes with the most basic of daily activities, including chewing, eating and talking. It’s exciting that Newcastle is leading much-needed research in this area, testing traditional tablet treatments against newer injectable treatments, including muscle relaxant Botox.
A reported 2 million people in the UK getting toothache a year. And yet, when a patient sits down and says they’re suffering with this type of pain, as a dentist your heart sinks.
Dialling down the pain volume after tooth treatment
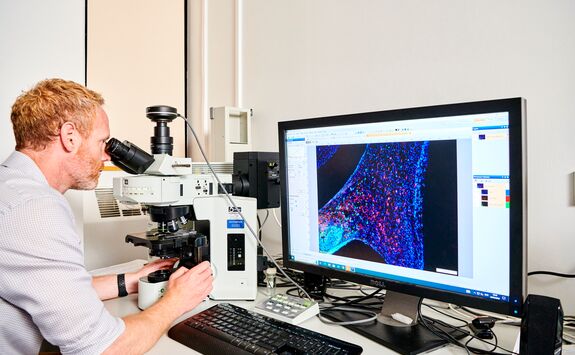
Another way we’re hoping to tackle tooth pain at Newcastle is by developing a novel cellular model that we can use as a testing ground for different medications to prevent and manage phantom tooth pain, tracking how it affects the signals sent to the brain’s pain receptors.
Phantom tooth pain – also known as atypical odontalgia or neuropathic orofacial pain – is a real pain, but caused by the pain system not ‘resetting the volume’ after the area has healed following a tooth or nerve removal. This could be because of over-sensitised and excited nerves in the area and in the brain creating a constant 7/10 pain on the pain scale for the patient. Phantom tooth pain occurs in 1.6% of people following toothache, extraction or root canal treatment, and can be lifelong.
The project, led by Dental graduates Dr Jamie Coulter and Emma Beecroft as part of Emma's PhD research, is in its early stages and has been supported by some generous fundraising from a patient with phantom tooth pain, who is crowdfunding £10,000 to support Emma’s research (details on how you can support this fundraising are below).
“Having lived with chronic toothache for the past two years—and facing the possibility of dealing with it for the rest of my life—it's incredibly encouraging to see the work that Emma and Jamie are doing. In a field where hope is often hard to find, their research for treatments for atypical odontalgia offers a rare and meaningful source of it. I hope the money I am raising can really help the dental pain community.”
James, patient and fundraiser
The money raised will help the team culture neurones in a lab that they can test different medications on to see how the pain receptors behave. They’ll be testing already approved medications for different conditions, that show promise in targeting right inflammatory processes to combat phantom tooth pain. It builds on the research I conducted for my own PhD, where I tracked the mechanisms going from the tooth to the brain to see how treatment – drilling out the inflamed nerve- affects the pain signals.
While £10,000 is a lot of money, it doesn’t stretch far in research sadly (a single antibody costs us £450!) and so this patient’s fundraising will help us run a pilot of the cellular model to test repurposed medications which we can hopefully then use to apply for grant funding to expand the project. The model being developed by Emma is the first of its kind worldwide, and if successful, will have many applications.

The model being developed is the first of its kind worldwide, and if successful, will have many applications.
Do the current ‘quick fixes’ fix anything?
While this research is ongoing, I’ve been researching the current ‘quick fixes’ offered to patients to see how different treatments lead to different outcomes (or not!)
My cohort study followed people from our out-of-hours service, emergency clinic and primary care who all presented with a raging toothache and had the whole or part of the nerve removed. Following this treatment, which is the only one available in a 20-minute NHS appointment if the patient wants to keep the tooth, 75% of dentists then add Ledermix paste, an antibiotic and steroid dressing, into the tooth.
25% of dentists don’t add Ledermix, as there’s evidence the antibiotics can leech out of the tooth, and we obviously don’t want to be using antibiotics if we don’t have to. We in the Endodontics team at Newcastle didn’t believe this paste was doing much to improve patient outcomes either, so around a decade ago we began teaching students here to dress with calcium hydroxide instead.
At the end of my study, I discovered that 1 in 4 patients were coming back within a week because they were still in so much pain, whatever dressing was applied. So this proved there was no clear impact with either of these ‘fixes’!
These results were the driver for the current research project we’re establishing. It painfully revealed that, as a sector, we are not good at dealing with tooth pain. I’m excited to see the results of the MiTiGate Trial and hope that we can get the cellular model approved for wider use to test new treatments.
Alongside these research projects and my teaching, I made headlines recently for performing a pioneering procedure on Rico the sloth at Chester Zoo. It’s for this I’ll probably be most remembered!
How you can get involved
If you are currently suffering from TMD – jaw muscle pain – we are still looking for patients to get involved in the MiTiGate trial of new and existing treatment.
You can also help contribute to our pilot project by donating to James' fundraiser via the link below.
