new skin cancer treatment
New therapy to overcome treatment-resistant skin cancers
Published on: 2 June 2025
A study has revealed why some patients don’t respond to immune checkpoint blockade (ICB) therapy for solid cancer tumours and identifies a new combination treatment.
New therapy to overcome treatment-resistant skin cancers
A study has revealed why some patients don’t respond to immune checkpoint blockade (ICB) therapy for solid cancer tumours and identifies a new combination treatment.
Publishing in Nature Immunology, the international group of experts led by scientists at Newcastle University, UK has identified the biological mechanisms leading to a revolution in our understanding of ICB resistance.
They identify a new combination strategy for treating ICB resistant metastatic skin cancers and suggest that this can also be of benefit in the immunotherapy treatment of other solid cancers.
Dr Shoba Amarnath, Reader in Immune Regulation at Newcastle University led the research. She says: “Identifying this mechanism is important as it identifies patients who will not respond to single agent ICB treatment such as anti-PD1 antibody therapy, but are most likely to benefit from the new combination therapy that we have identified, anti-CD30.
“By simply adding anti-CD30 for these patients, we can improve their response to cancer and avoid costly delays.
“Although our work was limited to skin cancer, we believe this new combination treatment will also benefit patients with lung, bowel, pancreatic and other solid cancers who are currently not responding to treatment with ICB monotherapy.”
ICB
The use of immune checkpoint blockade (ICB) therapy in solid cancers has shown unexpected success in a significant minority of patients. However, resistance to ICB therapy affects more than 60% of cancer patients who are prescribed this medicine. These medicines are expensive and cause significant toxicity in non-responders.
ICB therapy, or immune checkpoint blockade, is a type of immunotherapy that aims to unlock the body's natural immune system to attack cancer cells. It works by targeting and blocking specific "checkpoints" in the immune system that normally help to keep it in check, allowing T cells to recognise and destroy cancer cells more effectively.
ICB resistance understood
The scientists demonstrate that ICB resistance occurs due to their effect on a type of immune cell called T regulatory cells (Tregs). Selective blocking of the ICB protein PD-1 on Tregs alone paradoxically enhances cancer growth in these patients. They studied this using a new mouse model where PD1 deficiency was limited to Treg cells together with samples from human skin cancer patients to study ICB resistance. This new mouse was engineered by scientists at Newcastle University to specifically allow understanding of ICB resistance.
They found ICB therapy enhances the expression of several alternate checkpoint proteins in Tregs that drives enhanced cancer growth. In the paper they describe how targeting one of these immune suppressive proteins called CD30, can rescue, or overcome, checkpoint therapy resistance in skin cancer. As an opportunity for future study, an immunotoxin (an anti-CD30 immunotoxin, Brentoximab Vidotin; BV) targeting this protein is already available for treatment of blood cancers and the team believe this has potential as a combination therapy for other solid cancers.
There is also a significant development from a Phase II trial in the USA in patients who do not respond to ICB monotherapy. In the trial, combining anti-PD1 ICB and BV shows 24% median survival for refractory metastatic cutaneous melanoma, a melanoma that has spread to other parts of the body and is not responding to standard treatments. This provides a significant lifesaving alternative for late stage skin cancer patients who do not respond to standard ICB regiments.
Dr. Amarnath added: “Further progress in the laboratory has discovered new immune specific proteins and tumour growth proteins that have elevated expression in Tregs during ICB therapy. We also found that these Tregs show stem-cell like properties.
"Ongoing work in the laboratory includes understanding the function and potential therapeutic value of targeting these new proteins in Tregs in skin and other solid cancers.
“We are very excited to find all these new aspects in ICB resistance biology which will not be possible without this new murine model. We believe targeting immune molecules and tumor growth proteins, will significantly enhance the efficacy of ICB in solid cancers”.
Funding for the study came from RCUK, Medical Research Council (MRC), LEO Foundation, Academy of Medical Sciences, the National Centre for the Replacement Refinement and Reduction of Animals in Research (NC3Rs) and the National Institute for Health and Care Research (NIHR) Newcastle Biomedical Research Centre (BRC).
Reference: PD-1 receptor deficiency enhances CD30+ Treg cell function in melanoma. Nature Immunology. Shoba Amarnath: Newcastle University. DOI: 10.1038/s41590-025-02172-0
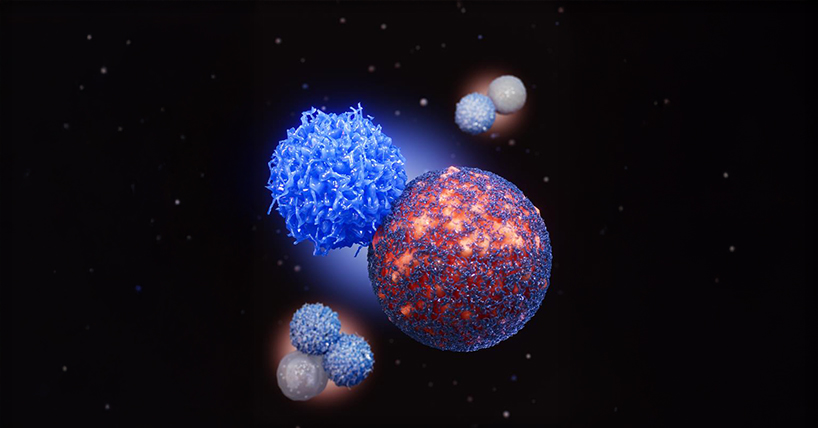
Picture caption: PD-1 deficiency enhances Treg cell pro-tumor function : Lim et al. demonstrate that Treg cells deficient in PD-1 occupy key spatial niches within the TME, with regulatory subsets organized near tumor cells dampening anti-tumor immunity (red and dark blue indicating a tumor protected by Treg cells), while cytotoxic (medium blue; red diffuse glow) and type 1 Treg cells (light blue; red diffuse glow ) are organized around immune cells driving active immune hubs.