Brain tumours are the most common cause of death from cancer in childhood. We carry out biological discovery to deliver the next generation of improved brain tumour therapies.
We run a multi-disciplinary, translational research programme. This brings together a wide-range of expertise, from basic biological studies to international clinical trials.
Our work focuses on two of the major high-risk brain tumour types of childhood:
- medulloblastoma: The most common malignant paediatric brain tumour
- atypical teratoid rhabdoid tumour (ATRT): A commonly lethal tumour type which arises most often in the first year of life
Together, these diseases account for over 300 childhood deaths every year in Europe.
Our principal approach to both tumour types is to understand their critical molecular features in detail. We use advanced next-generation genome-wide genetic and epigenetic technologies, alongside whole-tumour and single-cell analyses.
We use collections of primary and relapsed tumours linked to national and international clinical trials. We also use functional genomic models. We create these models to further understand their role in disease biology.
Translational strategies help us to develop biomarkers. We use the biomarkers to personalise therapy through better diagnosis, classification and prediction of disease course.
We apply this understanding to develop novel therapies targeted against specific disease biology.
We use equivalent strategies to understand the long-term side-effects associated with childhood brain tumours and their therapy, and develop interventional strategies.
We test our ideas and bring them into routine clinical practice through leading international clinical trials.
Tumour types
Medulloblastoma: We identify the molecular basis of medulloblastoma, variation between tumours, and its clinical relevance. We seek to understand intratumoural heterogeneity and its role in disease temporal evolution and relapse.
We model high-risk molecular features identified and exploit them in new therapeutic approaches.
ATRT: Major initiatives include first molecular characterisation of SMARCB1-dependent biology and its therapeutic relevance.
We're developing a detailed molecular pathological understanding of all malignant rhabdoid tumours of childhood. We're assessing their potential for clinical exploitation.
Area 1: Biomarkers, personalised therapies and molecular diagnostics
We discover and develop medulloblastoma biomarkers through our Cancer Research UK-funded biomarker research programme.
We use these to direct individualised therapies in pan-European clinical trials. We do this through our leading roles in trials design and associated biological studies.
We use these biological profiles to reduce treatment intensity for patients with good-risk disease. We develop new strategies for high-risk patients.
We aim to maximise cure rates while minimising long-term treatment side-effects.
The National medulloblastoma reference centre is based here in Newcastle. This delivers real-time molecular diagnostics for clinical trials and routine practice.
success stories:
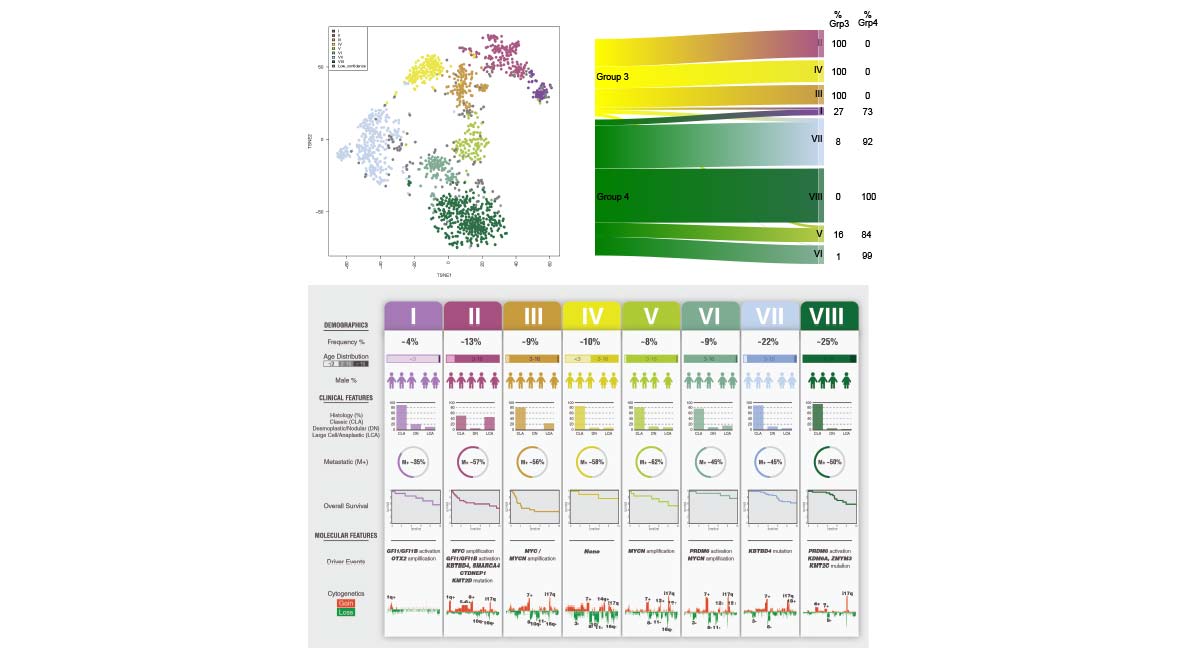
We discovered novel clinically-significant biological subtypes of medulloblastoma in 2017 using genomic and epigenomic investigations of large numbers of patients’ tumours. Our subsequent analysis in 2019 reached international consensus on the number and nature of these subtypes, and they will form the basis of the WHO 2021 sub-classification of medulloblastoma.
Area 2: Functional discovery and targeted therapeutics
We aim to understand the biological function of critical targets. We seek to exploit these in new therapeutic approaches.
We bring together:
- integrated tumour-based studies
- advanced functional genomic screening
- mouse modelling
- pre-clinical and early-clinical evaluations in high-risk brain tumours
We build our activities around our multi-institutional programme grant, INSTINCT (The Newcastle University – Institute for Cancer Research – Institute of Child Health High-risk Childhood Brain Tumour Network). This allows us to join brain tumour research expertise at:
- Newcastle
- Great Ormond Street Hospital / University College London
- The Royal Marsden Hospital / Institute of Cancer Research
success stories:
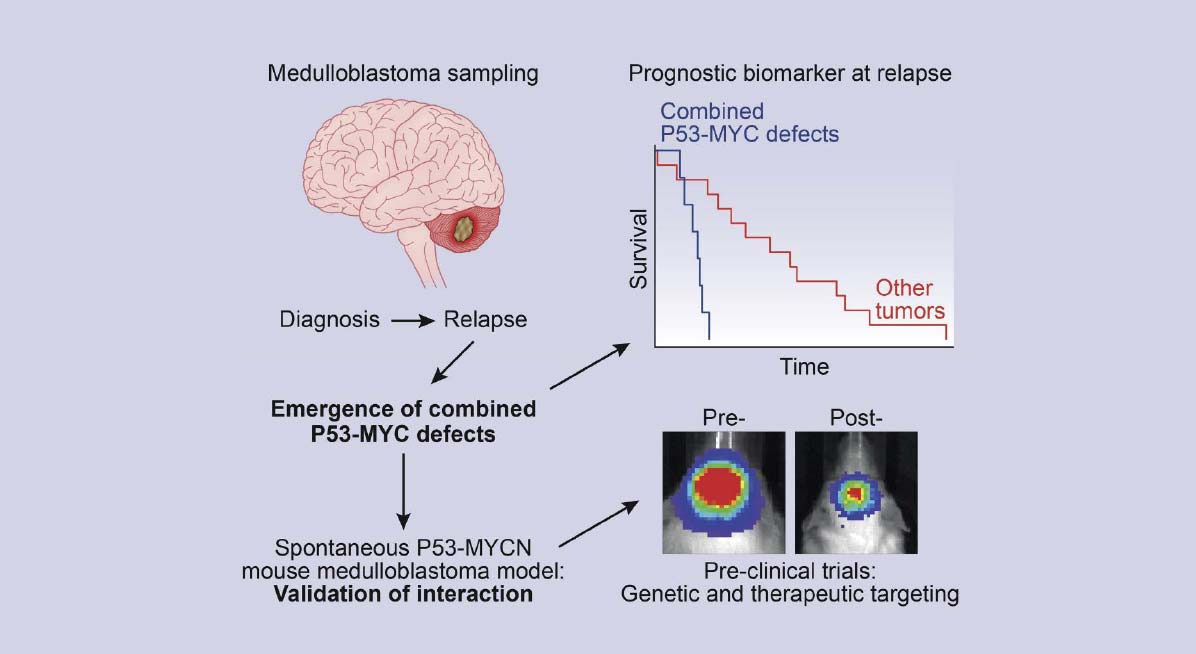
Our ground-breaking study in 2015 demonstrated that biology was significantly altered at medulloblastoma relapse with emergence of key drivers of disease discovered in a significant proportion of patients.
Crucially, these emerging drivers were clinically important: they predicted rapidly progressive disease after relapse, and could be therapeutically targeted in our modelling systems, reducing tumour growth and prolonging survival.
Our study provided first insights into the biological mechanisms driving relapsed medulloblastoma, offering promise that these mechanisms are predictable and targetable therapeutically.
Area 3: Survivorship
Medulloblastoma survival rates have plateaued at 60-70%. Furthermore, most survivors experience detrimental life-long late-effects associated with their disease and therapy. These ‘late-effects’ are life-changing and wide-ranging. The impacts extend into patients’ families, support networks, and the healthcare system over many life-years.
We have developed approaches to improve risk-stratification, sub-classification, and diagnostics/therapeutics of medulloblastoma to bear on survivorship outcomes.
Our research programme aims to reduce the disease- and therapy-associated late-effects burden in medulloblastoma survivors, through:
- understanding their nature and underlying biological mechanisms
- delivering less toxic, risk-stratified, curative treatments, based on this understanding
- developing personalised drug and rehabilitation interventions
Success stories:
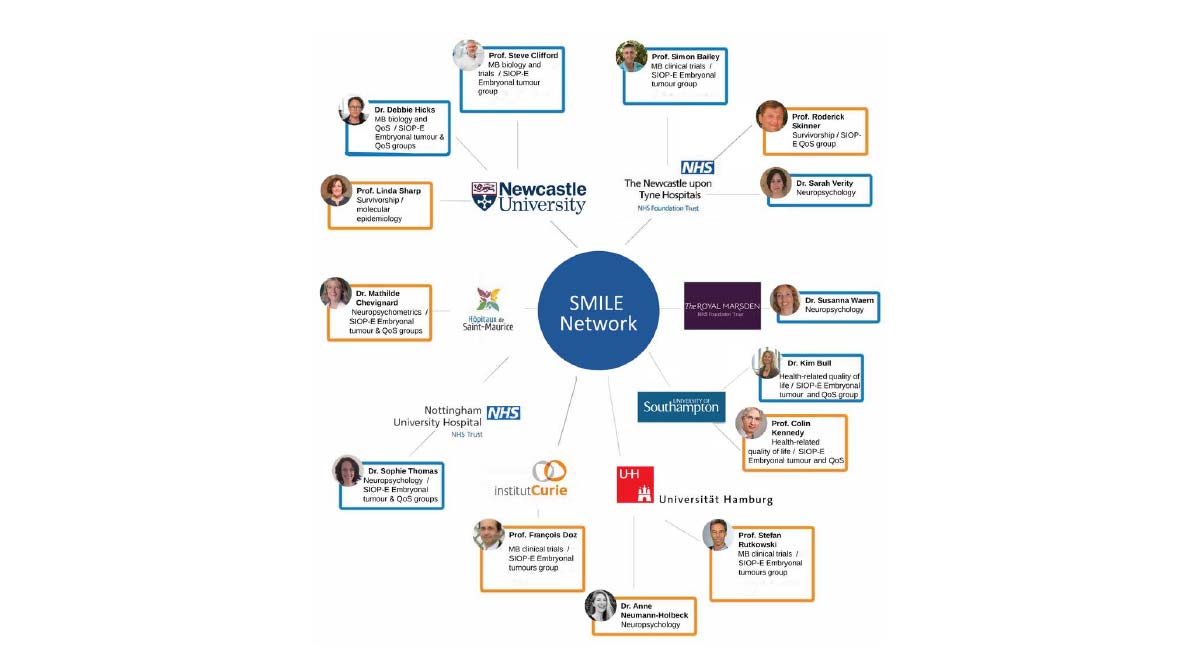
We have developed SMILE, an International network for Medulloblastoma Survivorship and Late-Effects, a unique multidisciplinary team of internationally leading experts and future leaders. Through SMILE, we are optimally positioned to advance medulloblastoma survivorship research and its translation into improved patient outcomes.
Area 4: Bioinformatics and resources
Our research programme is underpinned by expertise and capabilities in bioinformatics and genomics.
Our team of bioinformaticians is dedicated to childhood brain tumour research.
We have the high-performance computing resources and infrastructure necessary to perform high-throughput genomics.
We collaborate with INSTINCT partners. We make available our scripts and code and build open-source machine-learning classifiers implemented as web apps. This supports the molecular diagnostic and translational research community.
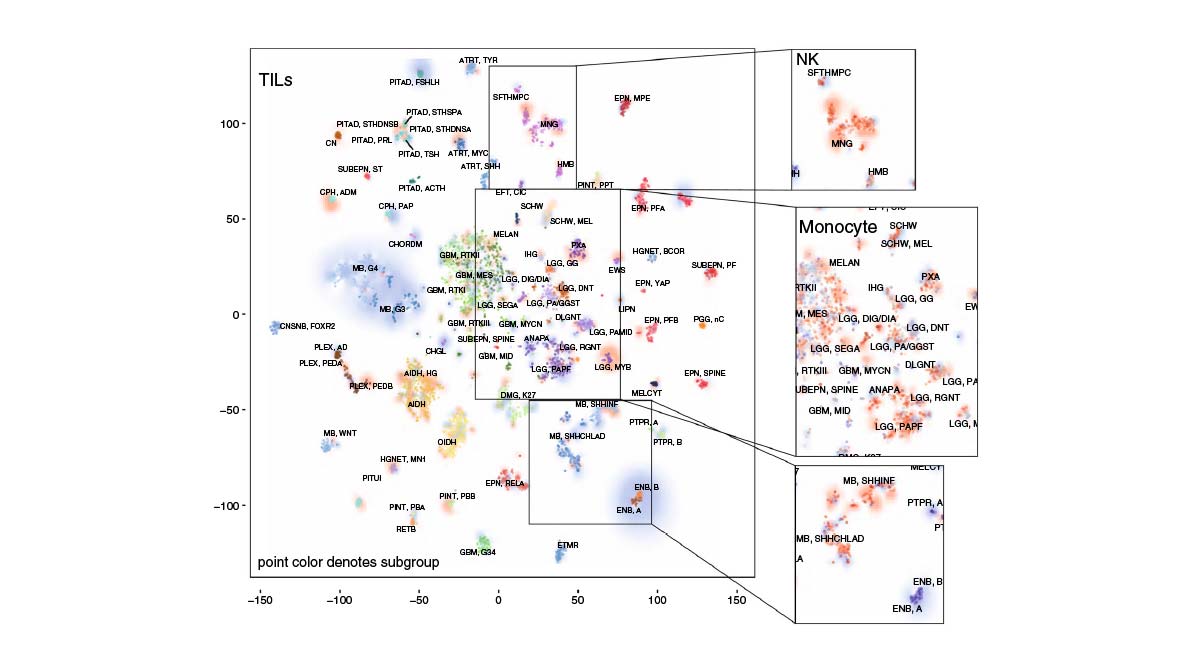
We used DNA methylomic profiling and bioinformatic approaches to investigate the constituency of the Tumor Immune Microenvironment (TIME) in >6000 primarily pediatric CNS tumors. Tumours grouped into three broad immune clusters associated with CNS tumor types, subtypes and prognosis, highlighting potential future therapeutic and prognostic possibilities to inform approaches to immune-therapy.
Area 5: Clinical trials
We lead on national and international clinical trials to test our clinical hypotheses and develop our research findings into routine clinical practice.
Our research programme has underpinned the delivery of biologically-directed risk stratified international trials for children with medulloblastoma, working as part of the International Society for Paediatric Oncology (SIOP-Europe) Brain Tumour group. Through these trials, biomarker discoveries from our team have been incorporated into the World Health Organisation (WHO) classification of medulloblastoma and are now in routine everyday clinical practice.
On behalf of SIOP-E, we have led biological research investigations within the SIOP-UKCCSG-PNET3 (1990-2000), HIT-SIOP-PNET4 (2000-2006) and the current SIOP-PNET5MB (2014-present) clinical trials. The international high-risk medulloblastoma trial opened in 2020 and is led by the Newcastle team.
We lead national interventional trials aimed at reducing the long-term side-effects of disease and treatment in medulloblastoma survivors.
Success stories:
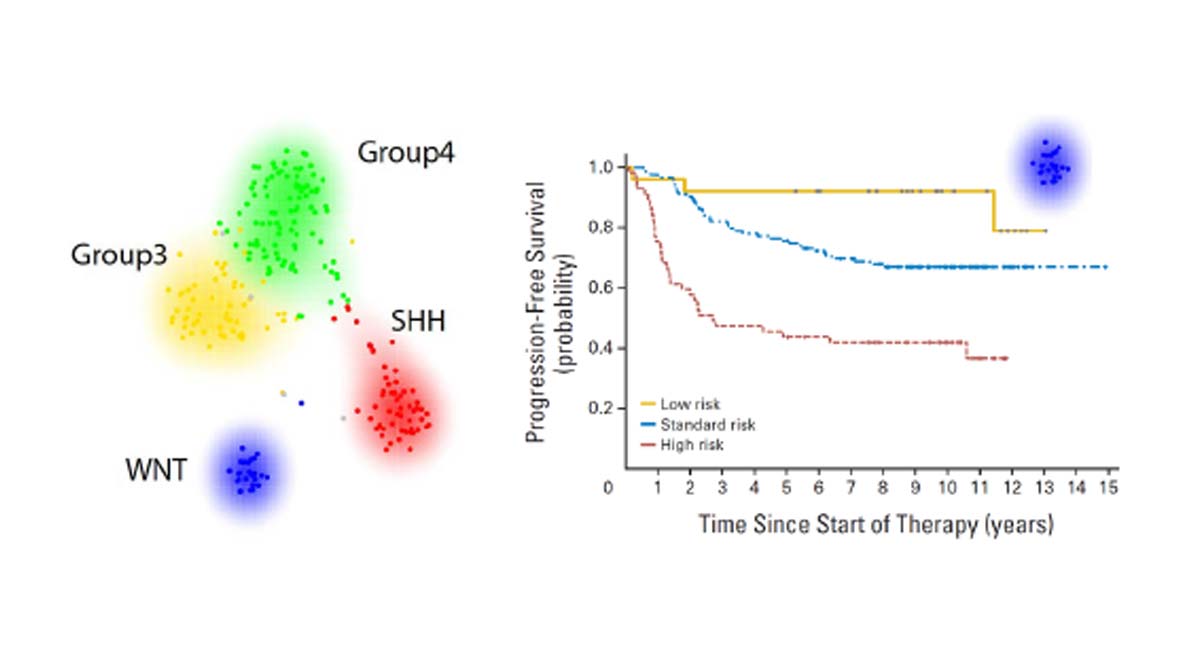
Our discovery of the WNT subgroup of medulloblastomas, associated with almost 100% survival, forms the basis of clinical trials of personalised medicine around the world. These trials are pioneering reduced therapies for WNT patients, aimed at reducing treatment intensity, duration and side-effects, while maintaining excellent survival rates.

.jpg)
.jpg)